For years, the cornerstones of cancer treatment have been surgery, chemotherapy, and radiation therapy. And now excitement is growing for immunotherapy–therapies that harness the power of a patient’s immune system to combat their disease.
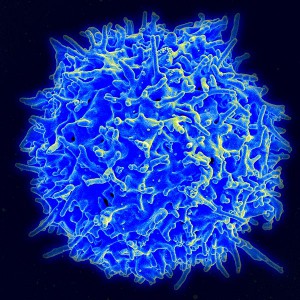
Healthy human T cell. By NIAID/NIH, via Wikimedia Commons
One approach to immunotherapy involves engineering patients’ own immune cells to recognize and attack their tumors and is called adoptive cell transfer (ACT). ACT’s building blocks are T cells, a type of immune cell collected from the patient’s own blood. After collection, the T cells are genetically engineered to produce special receptors on their surface called chimeric antigen receptors (CARs). CARs are proteins that allow the T cells to recognize a specific protein (antigen) on tumor cells. These engineered CAR T cells are then grown in the laboratory until they number in the billions. The expanded population of CAR T cells is then infused into the patient. After the infusion, if all goes as planned, the T cells multiply in the patient’s body and, with guidance from their engineered receptor, recognize and kill cancer cells that harbor the antigen on their surfaces.
Treatments with engineered immune cells have generated excellent responses in patients with advanced cancer.
Drs. Stanley Riddell, David Maloney and Cameron Turtle from Fred Hutchinson Cancer Research Center have contributed important discoveries about precisely how to use T cells for cancer therapies. A recent clinical trial using an advanced form of CAR T-cell therapy in patients with B-cell acute lymphoblastic leukemia, non-Hodgkin’s lymphoma and chronic lymphocytic leukemia has shown promising, even dramatic responses.
Fred Hutch’s Dr. Stan Riddell and colleagues are making significant strides in this exciting field, and continue to refine ways to use the human immune system to overcome cancer and other diseases. Video source: Fred Hutchinson Cancer Research Center
In the CHOP trial, all signs of cancer disappeared in 27 of the 30 patients treated in the study.
In several early-stage trials testing ACT in patients with advanced acute lymphoblastic leukemia (ALL) who had few if any remaining treatment options, many patients’ cancers have disappeared entirely. Several of these patients have remained cancer free for extended periods. In the CHOP trial, which is being conducted in collaboration with researchers from the University of Pennsylvania, all signs of cancer disappeared (a complete response) in 27 of the 30 patients treated in the study, according to findings published October 16 in the New England Journal of Medicine. Nineteen of the 27 patients with complete responses have remained in remission, the study authors reported, with 15 of these patients receiving no further therapy and 4 patients withdrawing from the trial to receive other therapy. Equally promising results have been reported in several small trials involving patients with lymphoma and in other similar studies (1-5).
Immunotherapy may represent a much-needed new option for patients whose cancers return after intensive chemotherapy or a stem cell transplant as the remaining treatment options are “close to none”.
Stephan Grupp, M.D., Ph.D., CHOP
CAR T-cell therapy can cause several worrisome side effects, perhaps the most troublesome being cytokine-release syndrome. The infused T cells release cytokines, which are chemical messengers that help the T cells carry out their duties. With cytokine-release syndrome, there is a rapid and massive release of cytokines into the bloodstream, which can lead to dangerously high fevers and precipitous drops in blood pressure.
For most patients, trial investigators have reported, the side effects are mild enough that they can be managed with standard supportive therapies, including steroids. Cytokine-release syndrome is a common problem in patients treated with CAR T cells. In the POB and CHOP trials, patients with the most extensive disease prior to receiving the CAR T cells were more likely to experience severe cases of cytokine-release syndrome.
Despite the success there is still much to learn about CAR T-cell therapy. However as dr. Rosenberg wrote in a Nature Reviews Clinical Oncology article, CAR T-cell therapy eventually may “become a standard therapy for some B-cell malignancies” like ALL and chronic lymphocytic leukemia.
Several other trials testing CAR T cells in children and adults are ongoing and, with greater interest and involvement from the pharmaceutical and biotechnology sector, more trials testing CAR T cells are being planned. Based on the success thus far, several research groups across the world are turning their attention to developing engineered T cells for other cancers, including solid tumors like pancreatic and brain cancers.
By Jana Erjavec, PhD, BioSistemika LLC
Further reading:
- Efficacy and toxicity management of 19-28z CAR T cell therapy in B cell acute lymphoblastic leukemia.
- Treating B-cell cancer with T cells expressing anti-CD19 chimeric antigen receptors.
- Chemotherapy-refractory diffuse large B-cell lymphoma and indolent B-cell malignancies can be effectively treated with autologous T cells expressing an anti-CD19 chimeric antigen receptor.
- Fred Hutch Clinical Trials
- Engineering T Cells for Safe and Effective Cancer Immunotherapy
Fred Hutchinson Cancer Research Center











